About Open-Angle Glaucoma
Chronic open-angle glaucoma is the most common form of glaucoma in the United States. The risk of developing chronic open-angle glaucoma increases with age. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve becomes sensitive even to normal eye pressures and is at risk for damage. Treatment is necessary to prevent further vision loss.
What Causes Open-Angle glaucoma?
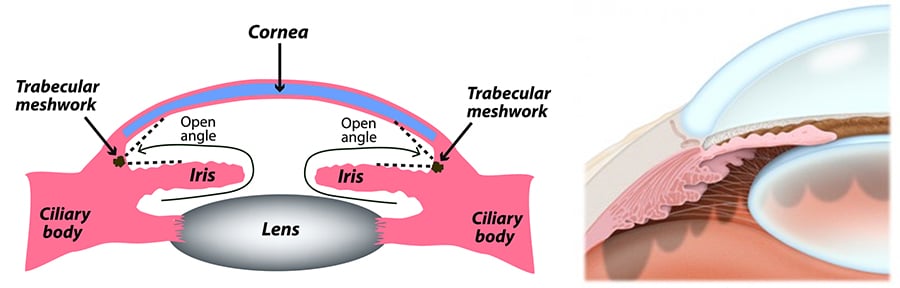
Our eyes have fluid inside them that keeps them healthy. This fluid changes with new fluid replacing the old, and the old fluid needs to exit the eye. That’s where the term “angle” comes in — there is a drainage angle formed by the cornea and the iris of your eyes. In this form of glaucoma, this angle remains open, but the trabecular meshwork through which the fluid drains has developed some sort of blockage, or your eye can be producing too much fluid and there is a backup in the outflow. Both of these situations cause the pressure to rise in your eye; this is open-angle glaucoma.
Open-angle is the more common form of glaucoma. This is different from closed-angle glaucoma where the iris bulges forward to narrow or block the drainage angle formed by the cornea and the iris.
Symptoms Of Open-Angle Glaucoma
Typically, open-angle glaucoma has no symptoms in its early stages, and vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in the field of vision.
You typically won’t notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. If all the optic nerve fibers die, blindness results.
Will Open-Angle Glaucoma Resolve On Its Own?
The main problem with open-angle glaucoma is that it presents few, if any, symptoms or warning signs before it has already caused permanent damage to the person’s vision. It is highly unlikely that it will go away on its own. More importantly, it’s definitely not worth the risk of waiting to find out. Glaucoma is the leading cause of blindness in Americans over the age of 60.
How Is Open-Angle Glaucoma Treated?
Once we’ve diagnosed a patient’s glaucoma, it’s important to quickly begin lowering the pressure inside the eye caused by the buildup of fluid. The goal is to prevent additional vision damage.
The first treatment option is prescription eye drops. Beyond that, surgery may be necessary to improve fluid drainage. These are the treatment options:
- Eye Drops — There are now a variety of different eye drop options for glaucoma treatment, depending on how your eyes respond. Some of these eye drops increase outflow of the aqueous fluid. Others seek to reduce production of fluid in the eye. Many people don’t comply with their dosages and the need for consistent application of their eye drops. This is the leading cause of continued damage to the optic nerve. This lack of urgency can be attributed to the fact that that the patient isn’t experiencing any pain or symptoms.
- Surgery — With surgery the goal is to improve fluid drainage within the eye.
- Laser Therapy: There are three options for laser surgery for glaucoma: laser trabeculoplasty, iridotomy, and cyclophotocoagulation. These procedures seek to increase outflow of fluid in the eye or to eliminate blockages in the trabecular meshwork.
- Filtering: In a trabeculectomy, part of the trabecular meshwork is removed to enhance drainage.
Drainage tubes: Small tubes are inserted, usually through the trabecular meshwork, to open flow.
- Minimally Invasive Glaucoma Surgery: These various techniques are used to lower eye pressure, generally with lower risk and easier recovery.
What To Do If You Have Open-Angle Glaucoma
There are some things you can do and not do to help to control high eye pressure with glaucoma. These are not in any way an alternative to the treatments described above from the team at Eye Care Institute.
- Eat a Healthy Diet — Several vitamins and nutrients are important for eye health, including zinc, copper, selenium, and the antioxidant vitamins C, E, and A.
- Exercise — Regular exercise can help reduce eye pressure.
- Limit Your Caffeine — Drinking too much coffee and other caffeinated drinks can increase eye pressure.
- Sip, Don’t Gulp — Drinking large amounts of liquids, amounts such as a quart or more, within a short time temporarily increases eye pressure.
- Sleep with your head elevated — It helps if you can raise your head to about a 20-degree angle when you sleep. A wedge pillow can do this.
- Be Consistent with Your Medication — Consistently use your eye drops and any other medications we prescribe for your open-angle glaucoma. Lackadaisical usage is the reason most people have continuing damage to their optic nerve. If there is one thing to be obsessive about doing, taking this medication would be it.
Open-Angle Glaucoma Risk Factors
Your ophthalmologist considers many kinds of information to determine your risk for developing this disease. The most important risk factors include:
- Age
- Elevated eye pressure
- Family history of glaucoma
- African or Hispanic ancestry
- Past eye injuries
- Thinner central corneal thickness
- Systemic health problems, including diabetes, migraine headaches, and poor circulation

Your ophthalmologist will weigh all of these factors before deciding whether you need treatment for glaucoma, or whether you should be monitored closely as a glaucoma suspect. This means your risk of developing glaucoma is higher than normal, and you need to have regular eye examinations to detect the early signs of damage to the optic nerve.
Can I Go Blind If My Open-Angle Glaucoma Goes Untreated?
As mentioned above, open-angle glaucoma is the leading cause of blindness in Americans over the age of 60. It is so dangerous because it shows few if any, signs before the increased pressure in the eye damage your optic nerve permanently. Most people have no idea they have glaucoma until damage has already occurred.
That’s why it is so important to have regular eye exams with the team at Eye Care Institute, especially after you pass your 40th birthday. If we don’t see you, or if we’ve found glaucoma but you’re lackadaisical about your use of your eyedrops, the outcomes are predictable. You will first lose your peripheral vision. Eventually, this will progress to tunnel vision, where you can only see objects directly in front of you. Continued untreated glaucoma will then lead to blindness in one or both eyes.
Are There Foods I Should Avoid to Manage Open-Angle Glaucoma?
If you're diagnosed with open-angle glaucoma, you may be advised to make some different lifestyle choices than you've made prior to having this condition. Because your eyes and general biology are different than anyone else's, your lifestyle modifications are unique to you. That said, there are some general types of foods that have consistently shown risks to eye health in people with open-angle glaucoma. This is because certain foods can affect intraocular pressure in some way. Examples of foods to avoid include:
- Caffeine. There is some evidence that caffeine can increase blood pressure, cholesterol, and intraocular pressure. Items like soda, dark chocolate, green tea, and coffee should be limited if not avoided altogether.
- Trans fats. These types of fat are found in a lot of the processed foods sold in grocery stores today. To avoid trans fats, limit or cut out potato chips, french fries and other fried foods, and packaged baked goods.
- Saturated fats. These types of fats can lead to weight gain and chronic health conditions like high cholesterol. Limit fatty meats as well as dairy products to minimize your consumption of saturated fats.
- Salt. Reducing salt intake can lower your blood pressure. As a result, your intraocular pressure may be easier to control using the treatments or medication prescribed to you.
Are There Activities I Should Avoid to Manage Open-Angle Glaucoma?
Exercise is an important aspect of maintaining optimal health. Regular physical movement helps lower a lot of the health conditions that can contribute to open-angle glaucoma, including high blood pressure and high cholesterol. That said, if you have elevated intraocular pressure that needs to be managed, the types of exercise and physical activities that you participate in must be approached with a great deal of discernment. You want your exercise routine to work for you not against you. Some of the activities that could increase intraocular pressure rather than decrease it include:
- Yoga. Some say that people with increased intraocular pressure should not do yoga. This isn't necessarily true in every case. If you have a yoga practice and are diagnosed with open-angle or closed-angle glaucoma, talk to your doctor and also your yoga instructor. With modifications, you may be able to continue your practice. In general, the step that's needed is to avoid all poses in which you're bent over. Downward dog, for example, is a pose that can send blood rushing to the head, increasing intraocular pressure.
- Weight lifting. You may be able to engage in some strength training exercises even with glaucoma. The concern is that lifting heavy weights, both during exercise or when performing tasks at home, can involve strain that increases the pressure on the optic nerve.
- Playing a wind instrument. Wind instruments like the saxophone or trumpet require you to push air in a more forceful way. The restriction in breathing can elevate the pressure in the face and head, resulting in too much intraocular pressure.
It's important to maintain an adequate level of physical activity if you have glaucoma. Some types of exercise are shown to decrease intraocular pressure post-workout. With this condition, you may walk, ride a bike, swim, and engage in many activities, even those that get you breathing heavy. The goal is to avoid activities during which you might hold your breath or strain in some way. If you have questions, your doctor can help you discern which activities are suitable.
Schedule an Open Eye Glaucoma Consultation
To learn more about Open Angle Glaucoma or to schedule an appointment with specialist, give us a call today at 707.546.9800 or fill out an online contact form and our office will be in touch with you. Our practice serves Santa Rosa, CA and the surrounding areas!